Click a link below to read more information about the procedure.
- Wrist Arthroplasty
- Keinböck's Disease
- Capitate Resurfacing
- 4 Corner Wrist Fusion
- Wrist Arthroscopy Tower
- Scaphoid Fractures
- Thumb Arthritis
- Distal Radius Fractures
- Triangular Fibrocartilage Complex Tears
- Carpal Instability
- SLIC Screw
- Hamate Fracture Excision
- Wrist Fusion
- Ulnar Abutment Syndrome
- Ganglions
- Hand Fractures
Total replacement of the wrist joint is less common than total elbow arthroplasty. This is because that there are many procedures that may be done on an arthritic wrist to help relieve pain and preserve motion that does not require joint replacement. However, in certain patients with severe bone deformity in low demand, a total wrist arthroplasty is an excellent indication. Patients with severe bone deformity secondary to rheumatoid arthritis are the most common indication. Frequently, these patients also may have involvement of the extensor tendons to the fingers with subluxation or potential rupture due to the form of the wrist joint. At the time of total wrist arthroplasty, the disorders of the finger extensors may be addressed at the same sitting.
The surgical technique involves an incision on the dorsum or back of the wrist. The extensor tendons are exposed and appropriate surgical management is performed if they are ruptured. Frequently, patients with severe deformity of the wrist also have involvement of the distal end of the ulna causing pain. This portion of the ulna may be removed or replaced in addition to the replacement of the radiocarpal joint. The wrist bones are exposed. The radius is replaced with a metal component shaped like the patient’s distal radius. The component fits down the medullary canal of the radius and is porous coated so the patient’s bone is able to grow into the prosthesis for stability. The carpal component is a metal back component with screws that fit into the carpus. A poly component is then attached to the carpal insert to adjust the patient’s range of motion and stability to the implant. The joint capsule is then closed. The procedure normally takes approximately 1 ½ - 2 hours. The patient’s wrist is immobilized for approximately three weeks. Range of motion to the finger and thumb is encouraged during that period of immobilization.
Physical therapy with range of motion and strengthening to the wrist is initiated at three weeks postoperatively. Patients usually notice a significant improvement in motion and pain relief by three months postoperatively. The advantage of total wrist arthroplasty is to help decrease patient’s pain, angular deformity, and range of motion so they can utilize their wrist in activities of daily living. Patients with total wrist arthroplasty normally would lead a sedentary-type life style to protect the implant. The biggest risk of total wrist arthroplasty is dislocation of the prosthesis and loosening of the distal component. With new designs in total wrist arthroplasty, these potential complications have decreased significantly.
Kienböck's disease is a relatively rare condition where the lunate bone of the wrist loses its blood supply. No one knows the exact cause of Kienböck's disease, but several theories have been put fourth including anatomic variations in some patients limiting the blood supply to the lunate, previous trauma, or repetitive micro-trauma disrupting the vascular supply. These are all theories.
Patients with Kienböck's disease present in various stages depending on how long the process has been going on. In earlier stages of Kienböck's disease, joint leveling or vascularized procedures are recommended in order to try either to take stress off the lunate bone, or to increase its blood supply.
In later stages, particularly Stage IIIB, the surgical options become more limited including partial wrist fusion, total wrist fusion, proximal carpectomy, or more recently pyrocarbon lunate replacement. A pyrocarbon lunate is an artificial lunate, which is man-made, in place of the necrotic avascular lunate bone. The advantage of this procedure, it helps replicate the patient’s normal anatomy, and does not burn any bridges if further salvage operations can be done in the future. Please see below Dr. Geissler’s technique video on pyrocarbon lunate replacement.
Patients who have a chronic ligament injury to the wrist can present with persistent radial sided wrist pain and swelling. The injury to the wrist may have occurred 15-20 years ago. Similarly patients may have had a fracture to the scaphoid, which is the most frequently fractured bone of the wrist, and if not treated can present with persistent radial sided wrist pain. Radiographs show arthritis to the wrist involving the radial scaphoid joint. Current treatment options for this degenerative arthritis to the wrist involving the radial side, involve proximal carpectomy which is removal of the proximal bones to the wrist, or partial fusion which means removal of the scaphoid and fusion of the remaining carpel bones. Proximal carpectomy has been a well-recognized procedure over the decades. It means removal of the scaphoid, lunate, and triquetrum which is the proximal row of bones to the wrist. The potential concern with this is the capitate is of a smaller diameter than the lunate fossa of the distal radius. Due to this mismatch, this can potentially cause arthritis to that joint due to the smaller capitate eroding into the bigger lunate fossa. One option to try to decrease this arthritis is capitate resurfacing. Another indication is end stage Keinbock’s Disease where the lunate has lost its blood supply and is necrotic and collapsed. In this procedure, the proximal row of bones is removed as previously, but the lunate fossa is anatomically measured. A capitate resurfacing implant is placed over the capitate to match the diameters of the lunate fossa in both the sagittal and coronal planes. The video below shows the capitate resurfacing procedure. In addition, a surgeon may add a soft tissue patch over the lunate fossa of the distal radius to add additional soft tissue protection to the joint surface.
Four-corner fusion is a partial fusion of the wrist bones in patients who have radio-scaphoid arthritis. The purpose of this procedure is to excise the scaphoid where the arthritis is and fuse the remaining carpal bones for wrist stability. Patients will retain approximately half the normal range of motion to the wrist. The goal is to decrease pain but also to maintain a functional range of motion to the wrist with preserved grip strength. This operation is considered in younger patients with wrist arthritis as compared to older patients who may option for a proximal row carpectomy.
Wrist arthroscopy has continued to evolve. As surgeons get more experience in it and new instrumentation develops, its popularity continues to grow. This is very minimal arthroscopic surgery for its disorders. Indications of wrist arthroscopy include scaphoid fractures, distal radius fractures, carpal ligament instability, tears of the fibrocartilage complex, and ganglions.
As shown above, wrist arthroscopy allows the surgeon an intraaticular view of the wrist under a bright light and in magnified conditions. This is the most sensitive and accurate way to evaluate the anatomy of the wrist. While magnetic resonance imaging (MRI) and plan x-rays can yield significant information, nothing is more sensitive than looking at the wrist joint directly through the arthroscope.
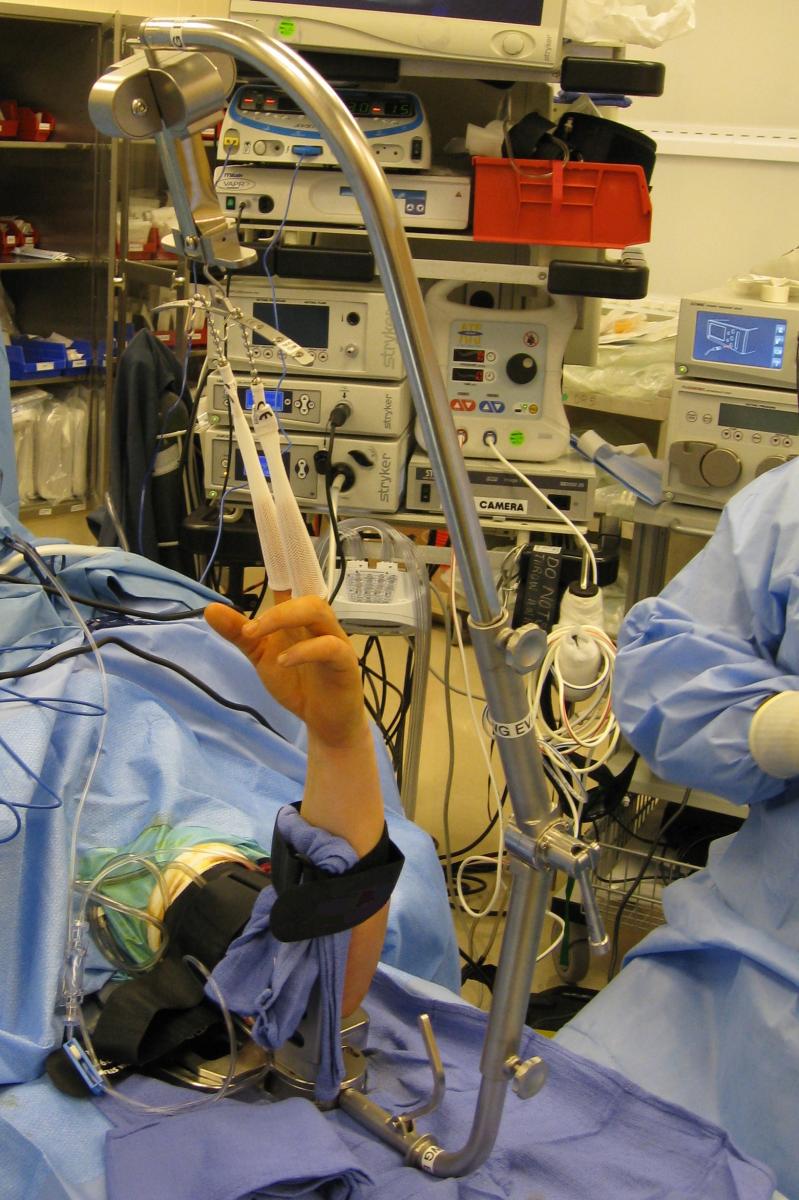
In the past, previous traction towers helped suspend the wrist, were not very functional for more advanced wrist arthroscopy procedures. Dr. Geissler was the sole surgeon designer of the Acumed Wrist Arthroscopy Tower. This tower is much different than previous towers on the market. The suspension bar runs along the side of the forearm rather than in front of it. This allows the surgeon to do more advanced arthroscopy techniques, such as arthroscopic distal radius and scaphoid fixation by allowing simultaneous arthroscopy and fluoroscopy. In addition, the arm of the tower flexes down, as some surgeons prefer to do wrist arthroscopy in a horizontal position, and others prefer to perform wrist arthroscopy in a vertical position. The tower has really allowed surgeons to do more advanced wrist arthroscopy as compared to previous towers on the market.



The scaphoid is the most common fractured carpal bone of the wrist. It generally occurs in young males between the ages of 15‑30. It is also a very common athletic injury which occurs in one in one hundred football players with a standing fracture of the scaphoid. Non-displaced fractures of the scaphoid will heal in a cast approximately 85‑90 percent of the time in review of the literature. However, patients may be in a cast for three months or longer to achieve healing. While one may achieve healing, they may be at risk of disuse atrophy to the muscles and bones of the hand and financial hardship of being in a cast for a prolonged period. For this reason, operative stabilization of both displaced and non-displaced fractures of the scaphoid have been advocated. The advantage of operative stabilization is the patient may start early range of motion without prolonged cast and immobilization following insertion of a screw. The fracture may be stabilized either arthroscopically or open.
Arthroscopic stabilization has several advantages with decreased scarring which potentially decreases loss of motion and is more cosmetic. In the procedure, two small portals are made on the posterior aspect of the wrist. With arthroscopic evaluation, a guide wire is placed down the central axis of the scaphoid through the posterior portal. Once confirmation of the guide wire is in ideal position, a headless cannulated screw may be placed over the guide wire across the fracture of the scaphoid. The headless screw fits all inside the scaphoid bone and does not need to be removed in the future as the bone heals. The advantage of the arthroscopic insertion is the ideal entry site can be seen arthroscopically and there is potentially decreased scarring as compared to open surgery.
Arthritis of the thumb carpometacarpal joint (CMC) is a very common problem. The thumb carpometacarpal joint is a uniquely shaped concave joint containing two saddle shaped bones that articulate perpendicular to each other. This allows for motion of the thumb in a number of different planes. This translation of the thumb metacarpal onto the trapezium in multiple planes can lead to arthritis of the carpometacarpal joint due to shear forces. This can lead to significant disability with pain at the base of the thumb with pinch and grip maneuvers.
Thumb carpometacarpal arthritis is mostly treated with non-surgical measures including splinting, medications, activity modifications, hand therapy, and intra-articular injections. When non-surgical methods or exhausted, there are multiple surgical options. These surgical options include volar ligament reconstruction, thermal shrinkage, arthrodesis of the thumb carpometacarpal joint, CMC joint arthroplasty, and trapeziectomy, which is removal of the trapezium.
In general, partial or complete removal of the trapezium is a standard procedure for this condition. Once the trapezium is excised, there are multiple methods described how to stabilize the thumb metacarpal so it does not translate proximally, after the trapezium has been removed. Techniques have been described from using a flexor tendon of the wrist (flexor carpi radialis), and some form of an internal brace. This includes a tight rope, forked anchors and more recently swivel lock anchors. The video below shows a new technique utilizing fiber tape and larger anchors (swivel lock) as the internal brace to suspend the thumb metacarpal to decrease proximal migration.
Displaced intraarticular fractures of the distal radius are the result of high energy injury. These fractures are less amenable to the traditional method of casting and immobilization. As the fracture extends into the joint, arthroscopic evaluation allows precise anatomic restoration of the joint surface under bright light and magnified conditions. The fracture may be stabilized by headless screws or may be stabilized by a plate and the articular reduction fine tuned arthroscopically to get the joint surface as anatomic as possible. The advantage of arthroscopic fixation allows precise anatomic restoration to the joint surface and identification of any additional soft tissue injuries that may occur with a fracture. Traditionally, fractures of the distal radius have been thought to be a bone injury. However, many studies show there is an additional soft tissue injury to the wrist ligaments. When this occurs, arthroscopic evaluation allows identification of these soft tissue injuries and stabilization at the same setting. In addition, arthroscopic lavage of the joint of bone debris and loose bodies may further improve the patient’s range of motion following this potentially severe injury. Dr. Geissler worked with Acumed to design a family of plates for volar, dorsal, and fragment specific fixation of these different injuries.
Triangular Fibrocartilage Complex Tears
The triangular fibrocartilage complex is a series of four structures about the distal radioulnar joint. The articular disk is a structure that connects the radius to the distal ulna and may be frequently torn. Patients usually sustain an injury to the triangular fibrocartilage complex through a sudden twisting motion to the wrist or a fall on the outstretched arm. A twisting injury such as using a power drill can result in a peripheral tear to the triangular fibrocartilage complex. The peripheral aspect of the complex is a blood supply and the tear can be arthroscopically repaired.
In this procedure, two small portals are made on the dorsum of the wrist. In a peripheral tear, a small incision may be made over the extensor carpi ulnaris tendon sheath and opened up. Sutures are then arthroscopically placed through the tendon sheath through the articular disk. In this soft tissue repair, the articular disk would be repaired back to the floor of the sheath of the extensor carpi ulnaris. This tissue has very good quality and has a very good secure repair. This technique takes approximately 30 minute to perform and is done as an out patient. Patients wear a splint over the elbow and wrist for approximately four weeks and a short arm splint for three weeks. Range of motion and strengthening are initiated at seven weeks postoperatively.
In patients who have instability to the distal radioulnar joint where the radius translates freely anteriorly and posteriorly, the peripheral tear of the TFC may be repaired back down to bone. In this manner, a small bone anchor is placed through a tiny incision over the head of the ulna. The sutures are then arthroscopically inserted through the articular disk and tied securing the disk back down to bone. This procedure takes approximately 45 minutes to perform on an out patient basis. The postoperative protocol is similar as described above.
Peripheral tears of the triangular fibrocartilage complex are a common problem. This results in pain about the ulnar side of the wrist when the patient twists the wrist like when opening a door or twisting the lid off a jar. Usually a twisting injury is a frequent mechanism of injury. It is also a very common athletic injury in patients with racquet sports or in baseball players.
The triangular fibrocartilage complex has two layers. The superficial layer can be seen relatively easy arthroscopically and then the deep layer called the ligamentum subcruetum. There are multiple ways to fix a peripheral tear of the TFC when it is torn, the majority of which leaves suture knots which can cause symptoms. Dr. Geissler worked with Arthex Corporation to devise an all arthroscopic knotless technique. This repairs both layers of the articular disk back down to bone with a knotless technique. This avoids irritation from suture knots, and in his experience, patients seem to regain their motion faster with less pain with this surgical technique.
The ligaments of the wrist are quite complex. With a fall on an outstretched arm, the ligaments have been shown to stretch and eventually tear. In most instances, the ligament tears from volar to dorsal. Dr. Geissler published an arthroscopic classification of wrist instability several years ago, which has been quoted worldwide for acute tears to the interosseous ligaments of the wrist. This classification defines specific management depending on severity of the tear. In acute partial lesions, partial tears to the interosseous ligaments usually involving carpal bones may be stabilized arthroscopically. Stabilizing the involved carpal bones across where the ligament tear occurs allows that tear to heal.
In patients who have chronic lesions to the interosseous ligaments, arthroscopic debridement or thermal shrinkage may be of benefit. Dr. Geissler presented his results of thermal shrinkage to chronic partial tears of the interosseous ligaments to the American Association of Hand Surgery. He noted that patients that had a partial tear that electro thermal shrinkage had good results in selected patients. In more severe deformities, traditional open reconstruction may need to be considered.
While acute partial tears of the interosseous ligament may be addressed arthroscopically, acute complete tears and chronic tears of the interosseous ligament are usually managed with open incisions. Frequently, Kirschner wires are used to hold the repair following reconstruction of the ligaments. These are wires that may be cut just below the skin or protrude through the skin. The disadvantages of Kirschner wires are that when they stick out of the skin, they can potentially get infected, have to be kept dry, and limit early rehabilitation. These wires are usually pulled about 6-8 weeks after insertion, and the ligament may not have had sufficient time of stabilization for complete healing. Patients are usually checked every few weeks for their pin tracts to make sure there is no infection requiring frequent office visits.
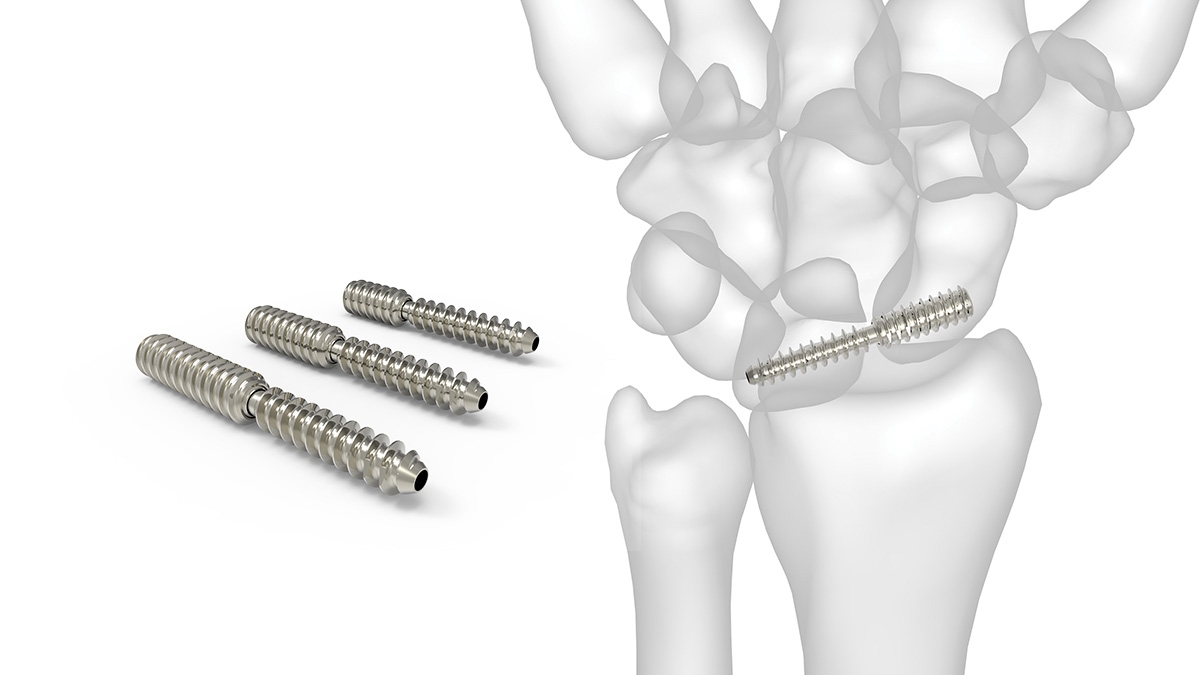
Dr. Geissler was the sole surgeon designer, working with engineers at Acumed to develop the SLIC screw (Scapho-Lunate Inter Carpal Screw). This screw freely rotates and toggles in the middle of its length. The goal is to place the screw across the involved carpal ligament tear, and stabilize the two bones while the ligament heals for a long period of time, usually 6-9 months. The screw can be removed at that point percutaneously, or left in depending on the patient’s preference. Since the screw rotates in the middle, this allows the carpal bones to rotate more naturally between themselves as compared to a solid screw, or Kirschner wires. Patients particularly can start earlier rehabilitation with the SLIC screw as compared to the traditional Kirschner wires.
Below is a picture of the SLIC screw, and videos describing its development and use.
Text Coming Soon
Wrist fusion (wrist arthrodesis) is usually used as a salvage procedure when previous wrist operations designed to relieve pain, but yet preserve motion, did not provide satisfactory results. A wrist fusion is a very dependable operation that significantly decreases or eliminates wrist pain, and leaves a very functional hand. A wrist fusion, allows the patient to continue to do quite heavy lifting. The disadvantage of a wrist fusion, is that it obviously takes away any motion of the wrist itself. The thumb and fingers will be mobile, but the wrist will not move. When a wrist fusion is performed, the wrist is usually positioned in slight extension to allow for maximum grip strength to the hand.
Previous wrist plates were basically straight and passed underneath the extensor tendons to the fingers to attach to the long metacarpal. While these were very functional plates, they frequently irritated the extensor tendons, and had to be removed later after the wrist had been fused. In addition, the screws were passed from posterior to an anterior direction leaving a potentially rough surface area causing further irritation to the extensor tendons.
Dr. Geissler was the sole surgeon designer, and worked with the engineers at Acumed to design a plate that actually was curved so that the plate attaches to the index metacarpal. In this manner, the plate is positioned away from the extensor tendons to decrease irritation. In addition, the dorsal surface of the plate is smooth and the screws come in from the side rather than directly posterior/anterior which is potentially a stronger construct compared to previous straight plates. In certain incidences, a surgeon may elect to place the plate on the long metacarpal underneath the extensor tendons. To address this, Dr. Geissler designed a plate that is straight, but smooth distally on top, so it help decrease irritation to the extensor tendons, and again the screws come in from the sides to cause less irritation to the tendons and to be a potentially stronger construct.
Ulnar impaction results when the ulna is longer than the radius. This can be from a normal congenital variant which occurs in approximately 20% of the population, or from a distal radius fracture that has healed shortened allowing the ulna to be more prominent. This dramatically shifts the load over to the ulnar side of the wrist increasing ulnar-sided pain. Patients complain of pain with grip and rotation of the forearm about the ulnar side of the wrist that radiates proximally toward to elbow.
Dr. Geissler devised a ulnar shortening plate specifically designed to shorten the ulna. This greatly simplifies the procedure. He previously published with his colleagues their results in 90 patients with 100% union rate and no metal removal. Previous plates, particularly, were symptomatic and had to be removed. While there is some potential for this plate to be removed, it is felt that the incidence of metal removal is lower as the plate is low profile and placed on the volar aspect of the ulna.
Patients with ulnar abutment syndrome have a condition where the ulna is longer in relation to the radius. Frequently, patients have a history of a previous radius fracture which has healed with some settling and shortening making the ulna longer in relation to the radius. In patients with ulnar abutment syndrome, patients particularly present with pain about the ulnar side of the wrist. They feel popping and catching to the wrist. It hurts to deviate the wrist toward the ulnar side of the forearm. In addition, it may hurt to pronate and supinate the forearm. Patients frequently have a central tear to the articular disk to the triangular fibrocartilage complex.
In this condition, the wrist is arthroscopically evaluated through two portals on the dorsum of the wrist. The central tear of the articular disk is débrided back to stable tissue. Patients also may have involvement of the lunotriquetral interosseous ligament more distally in the wrist. In ulnar abutment syndrome, the true pathology is the increased link of the ulna to the radius. For that reason, the ulna is then shortened so it is the same link or slightly shorter than the radius. In this procedure, Dr. Geissler uses the ulnar shortening plate that he designed with Acumed, LLC. An incision is made on the ulnar side of the forearm. A plate is placed on the volar aspect of the ulna so it is less symptomatic. By utilizing the plate, the surgeon can judge the exact amount of shortening to the ulna bone. A wafer of bone is removed and the ulna is shortened. The plate is quite stable and holds the fixation while the osteotomy site heals. The previous problem with ulnar shortening plates is that they were symptomatic and had to be removed a high percentage of time. This new ulnar shortening plate significantly decreases the complexities of the surgery and being a more lower profile rounded plate has significantly decreased the incidence of plate removal. This procedure is performed on an out patient basis and takes approximately 60‑90 minutes to perform. Patients are immobilized for one week and start range of motion exercises as tolerated.
A dorsal ganglion is the most common benign growth to the wrist. Patients notice a circular bump on the back of the wrist. Patients particularly complain of pain with terminal flexion and extension of the wrist due to the mass effect. Aspiration of the ganglion has approximately 30 percent success rate. If the ganglion reoccurs or the patients are unhappy with the cosmetic appearance of the ganglion, it may be excised. Ganglions may be excised either open or arthroscopically. The advantage of arthroscopic excision has potentially less scarring which will result in decreased wrist stiffness and wrist flexion.
In this procedure, two small portals are made on the dorsum of the wrist. One portal is made directly into the sac of the ganglion where it is arthroscopically excised. This procedure takes approximately 30 minutes to perform on an out patient basis. A dressing is worn for three days, then band aids will be placed over the two portals, and medial range of motion exercises are initiated. There are no restrictions.
Fractures of the hand involve one-third of all injuries involving the upper extremity. It is estimated that there are 1.5 million hand fractures a year resulting in 16 million lost work days. Fractures of the hand have special problems in fixation as these result in ultimately small fragments that are hard to control, the flexor and extensor tendons of the hand run against the bone, and this can result in tendon and joint adhesions secondary to the fracture. In general, patients are unable to tolerate implants for metacarpal fractures as compared to fractures of the phalanges (fingers). In this incidence, less is more. For the fingers, generally percutaneous pins or lag screws are preferred; however, in very comminuted fractures or multiple fractures, plate fixation may occasionally be required.
New Fracture Management Technique
Fractures that are displaced, frequently will require fixation. This will be either by plate or intrameduallary rod. Typically, provisional fixation is performed to temporarily hold the fracture in an anatomic position while the plate or rod is being inserted. This is usually performed with a separate lag screw or Kirschner wires. However this can get in the way of the final implant as it is being placed. The Geissler “Sling and Cinch” provides provisional fixation with fiber tape with low profile provisional fixation. This also allows the surgeon to anatomically reduce the fracture so the plate can be applied directly on top of the sling making it easier for the surgeon to stabilize the fracture. In addition, the surgeon can drill through the tape if necessary for the final implant. Below is a video of the Geissler “Sling and Cinch” for provisional fixation.